The Study to Understand the Genetics of the Acute Response to Metformin and Glipizide in Humans (SUGAR-MGH): Design of a pharmacogenetic resource for type 2 diabetes
OBJECTIVE:
Genome-wide association studies have uncovered a large number of genetic variants associated with type 2 diabetes or related phenotypes. In many cases the causal gene or polymorphism has not been identified, and its impact on response to anti-hyperglycemic medications is unknown. The Study to Understand the Genetics of the Acute Response to Metformin and Glipizide in Humans (SUGAR-MGH, NCT01762046) is a novel resource of genetic and biochemical data following glipizide and metformin administration. We describe recruitment, enrollment, and phenotyping procedures and preliminary results for the first 668 of our planned 1,000 participants enriched for individuals at risk of requiring anti-diabetic therapy in the future.
METHODS:
All individuals are challenged with 5 mg glipizide × 1; twice daily 500 mg metformin × 2 days; and 75-g oral glucose tolerance test following metformin. Genetic variants associated with glycemic traits and blood glucose, insulin, and other hormones at baseline and following each intervention are measured.
RESULTS:
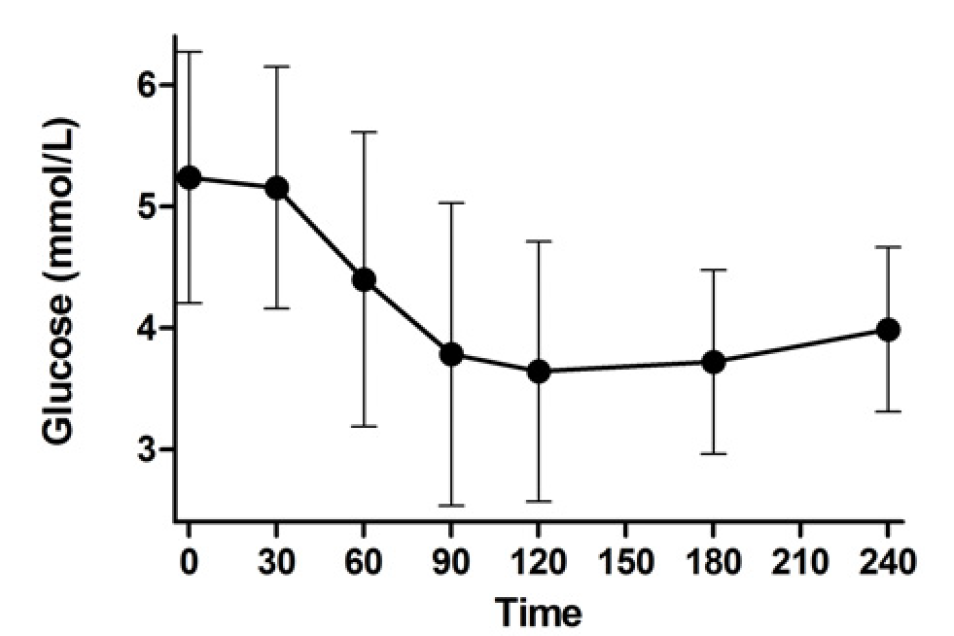
Approximately 50% of the cohort is female and 30% belong to an ethnic minority group. Following glipizide administration, peak insulin occurred at 60 minutes and trough glucose at 120 minutes. Thirty percent of participants experienced non-severe symptomatic hypoglycemia and required rescue with oral glucose. Following metformin administration, fasting glucose and insulin were reduced. Common genetic variants were associated with fasting glucose levels.
CONCLUSIONS:
SUGAR-MGH represents a viable pharmacogenetic resource which, when completed, will serve to characterize genetic influences on pharmacological perturbations, and help establish the functional relevance of newly discovered genetic loci to therapy of type 2 diabetes.